Unintended pregnancy in Delaware: Estimating change after the first two years of an intervention to increase contraceptive access
Authors
The United States has a high rate of unintended pregnancy. In 2011, nearly half (45 percent) of pregnancies nationwide were unintended (either unwanted or occurred sooner than desired).1 Researchers have found that births resulting from unintended pregnancies are linked to a range of negative health outcomes for women and children.2-4 Increasing the use of effective methods of contraception among sexually active women, especially long acting reversible contraception (LARC) methods such as the IUD and implant, can help reduce unintended pregnancy and improve maternal and child health outcomes.5-8
Upstream USA is a nonprofit whose mission is to change health care so that all women receive the highest quality services and have convenient access to the full range of contraceptive methods. In December 2014, Upstream introduced its first statewide initiative in Delaware. The organization is working in partnership with the governor and the Division of Public Health to implement Delaware Contraceptive Access Now (Delaware CAN). Delaware CAN is a comprehensive, statewide program to ensure all women in the state have convenient access to the birth control method of their choice. Upstream is providing training, technical assistance, and quality improvement activities to all publicly funded Title X health centers, the largest private providers, and five of the six hospitals in the state.
Upstream commissioned Child Trends to examine how contraceptive use among female family planning clients at Title X clinics in Delaware has changed during the implementation of Delaware CAN and to estimate, using the microsimulation model FamilyScape 3.0, how these changes in contraceptive use may have affected unintended pregnancy among this population. FamilyScape 3.0 is a microsimulation model designed to replicate fertility-related behaviors and outcomes among U.S. women of childbearing age. In the absence of pregnancy data for Title X family planning clients, FamilyScape 3.0 allows us to simulate changes in unintended pregnancy due to changes in contraceptive use.
We also compared the changes in contraceptive use and unintended pregnancy among women at Delaware’s Title X clinics to changes in contraceptive use and unintended pregnancy among Title X family planning clients nationwide. LARC use has increased in the last decade across the country,9 and we wanted to understand whether the findings for Delaware were unique or simply part of a nationwide trend. These analyses allowed us to assess whether and how the estimated declines in unplanned pregnancy in Delaware differed from those in the country as a whole.
Key Findings
Our analysis indicates that since Upstream’s implementation of Delaware CAN, there has been a substantial increase in LARC use and a small decrease in the use of no method among clients of Title X family planning clinics in Delaware. Simulations to model the effect of changes in contraceptive use indicate a substantial reduction in unplanned pregnancy among this population. Estimated trends in LARC uptake and decreases in unintended pregnancy among Delaware Title X family planning clients were much greater than those observed among clients nationwide.
- Among Delaware Title X family planning clients aged 20 to 39, there was an increase in LARC use from 13.7 percent to 27.0 percent between 2014 and 2016.
- The increase in LARC use was primarily offset by a decrease in hormonal methods such as the Pill, patch, and ring. There was also a small decrease in non-use of contraception (just under 2 percentage points).
- In Delaware, this movement from moderately effective methods to highly effective LARCs, paired with a small decrease in non-use, resulted in a substantial simulated decrease—of 15 percent—in the unintended pregnancy rate among this population, between 2014 and 2016.
- Similar analyses of changes in method use among Title X family planning clients nationwide found a smaller increase in LARC use—from 13.6 percent to 17.6 percent—and no decrease in non-use. The resulting simulated decrease in unintended pregnancy was 1.3 percent during the same period.
Background
Nationwide the unintended pregnancy rate is 45 per 1,000 women (aged 15 to 44). As of 2010 (the most recent data available), Delaware’s unintended pregnancy rate among all women 15 to 44 was even higher—62 per 1,000 women. In fact, Delaware had the highest unintended pregnancy rate in the country in 2010.10
Research suggests that unintended pregnancies are associated with adverse pregnancy-related behaviors such as smoking and delayed prenatal care.2 Births from unintended pregnancies are more likely to result in several critical challenges for babies, including low birth weight, which is associated with increased health challenges over the course of a child’s life.3,11
Almost all women who have unintended pregnancies failed to use contraceptives consistently or correctly, had extended gaps in birth control use, or often used no method at all.12 Efforts to expand the use of any birth control among women using no contraception, and to increase the use of highly effective methods (such as the IUD or implant, which have failure rates of less than 1 percent) among women relying on less effective methods of birth control, may lead to reductions in unintended pregnancy.
Upstream partners with states to provide training and technical assistance to health centers, including public health centers, private practices and hospitals, to ensure the availability of the full range of contraceptive methods. Upstream’s approach includes training to increase staff knowledge, confidence, and behaviors needed to provide single-visit access to all contraceptive methods, including LARCs; and on-site coaching on how to deliver high-quality, medically-accurate, patient-centered counseling.
To date, Upstream has trained and supported staff in 41 health care and social service agencies that serve 165 health care delivery sites and reach over 126,000 women of reproductive age annually in Delaware. Early results from Upstream’s internal monitoring data suggest that these health centers are improving the quality of contraceptive care. For instance, clinicians and support staff have increased knowledge of and confidence in LARC methods, clinic staff members include questions about pregnancy intentions in patient screening, and medical assistants often participate in contraceptive counseling. At Delaware clinics partnering with Upstream, 98 percent of patients surveyed reported that they did not feel pressured by staff at the health center to use a particular method and that they were involved in their own contraceptive method decision.a
a. Early results of Delaware CAN are currently unpublished and were provided to us by Upstream.
Data and Methodology
Child Trends used the FamilyScape model to estimate the effect of a change in contraceptive method use among Title X patients in Delaware on the unintended pregnancy rate. FamilyScape 3.0 is a microsimulation tool that allows the user to model the impacts of behavioral changes (e.g., an increase in the use of longacting reversible contraception) on critical family-formation outcomes. It realistically simulates the key antecedents of pregnancy (sexual activity, contraceptive use, and female fecundity) and many of its important outcomes (such as pregnancy and childbearing within and outside of marriage, children’s chances of being born into poverty, and abortion). FamilyScape is designed to reproduce real-world fertility-related behaviors; for instance, the model incorporates the typical-use failure and continuation rates for birth control methods (typical-use failure rates account for incorrect and inconsistent use, as opposed to theoretical perfect-use failure rates estimated during clinical trials).b
For our analyses, we employed data on the primary methods used by female family planning clients from Delaware’s Family Planning Annual Reports and from the national Family Planning Annual Reports for 2014, 2015 and 2016.13-15 The Delaware Department of Health and Social Services, Division of Public Health provided the Delaware data. We calculated contraceptive distributions among women aged 20 to 39. Contraceptive methods were grouped together per FamilyScape’s existing parameters (e.g., Pill, patch, and ring are combined into one category in FamilyScape). We limited our analysis to women aged 20 to 39 because FamilyScape less accurately predicts pregnancies to women aged 40 and older, and there were data quality issues with Delaware’s statewide Title X data for teen women (outlined in the “Limitations” section of this brief). We also excluded women who were missing information on their primary method. Approximately one third of women in our population of interest in Delaware over the three years studied were missing contraceptive method data (see “Limitations” for more details). Finally, we excluded women who were abstinent and women who were pregnant or seeking pregnancy. Because we limited our sample to women not seeking pregnancy, the failure rate of the no method category in the FamilyScape model was revised downward to 46 percent, which is the estimated average failure rate over one year for women using no method and not seeking pregnancy.16 Based on this, the pregnancy rates simulated by FamilyScape are considered unintended pregnancy rates among women at risk of unintended pregnancy.c
b. For more information on FamilyScape please visit https://childtrends.org/research/research-by-topic/familyscape-3-0-microsimulation-model/
c. This is distinct from other research that reports pregnancy rates and unintended pregnancy rates as the number of pregnancies or unintended pregnancies per 1,000 women in the population (not limiting to women at risk of unintended pregnancy).
Findings
Contraceptive distributions among Title X family planning clients in Delaware, 2014 to 2016
Over the three years studied, Title X family planning data indicate a large increase in LARC use among Delaware clients (Table 1). The percentage of women using a LARC increased from 13.7 percent to 27.0 percent between 2014 and 2016. This increase was offset by a similar decrease in the use of hormonal methods—the Pill, patch, or ring—from 35.8 percent of female family planning clients in 2014 to 23.4 percent in 2016. There was also a slight decrease in no method use, from 5.4 percent to 3.6 percent. We highlight this decrease because nationally, women who were using no method during the month of conception account for more than half of unintended pregnancies,17 so even a small shift in the proportion using no method can have a large impact on the unintended pregnancy rate.18 The percentage of women using sterilization, injectables, and condoms stayed relatively consistent over time.
Table 1. Contraceptive method distributions for Delaware Title X female family planning clients aged 20 to 39, 2014 to 2016
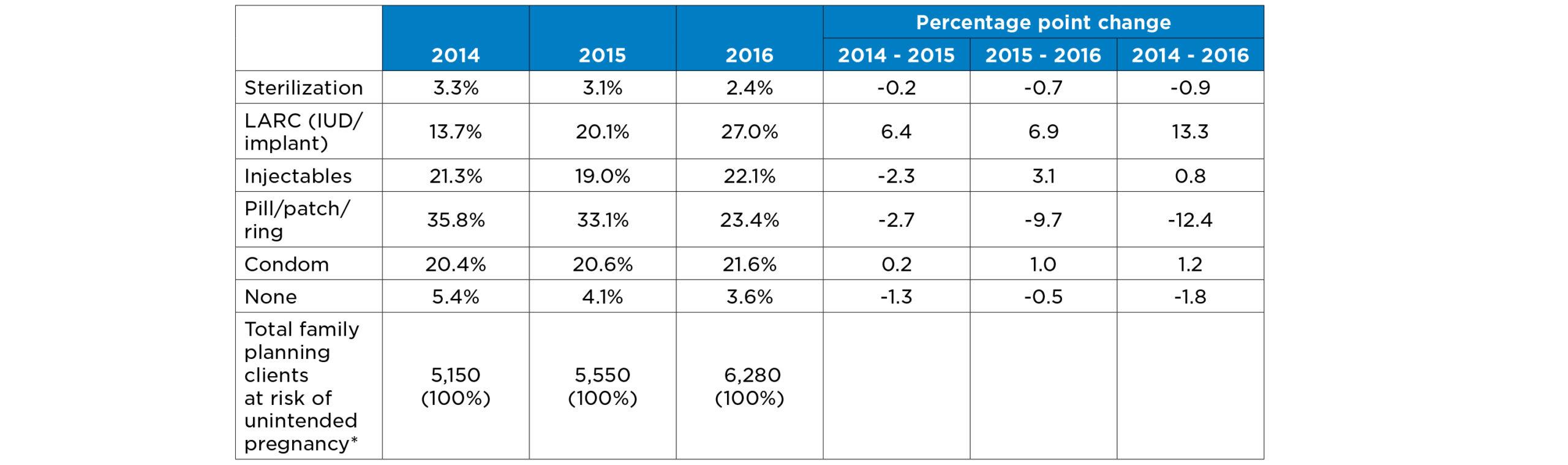
Source: State-level Title X data provided by Delaware Department of Health and Social Services, Division of Public Health
*We exclude women who were abstinent or pregnant/seeking pregnancy. We also exclude women whose method was categorized as Unknown: 43% of 20-39-year-olds at risk of unintended pregnancy in 2014 and approximately 27% in 2015 and 2016. Numbers are rounded to the nearest ten.
Contraceptive distributions among U.S. Title X Family Planning Clients, 2014-2016
Although less substantial than in Delaware, clients of Title X family planning sites nationwide also experienced an increase in LARC use, from 13.6 percent to 17.6 percent (see Table 2). This increase was offset by reductions in injectables and hormonal methods such as the Pill, patch, and ring. The use of other method types, and non-use, remained fairly constant.
Table 2. Contraceptive method distributions for U.S. Title X female family planning clients aged 20 to 39, 2014 to 2016
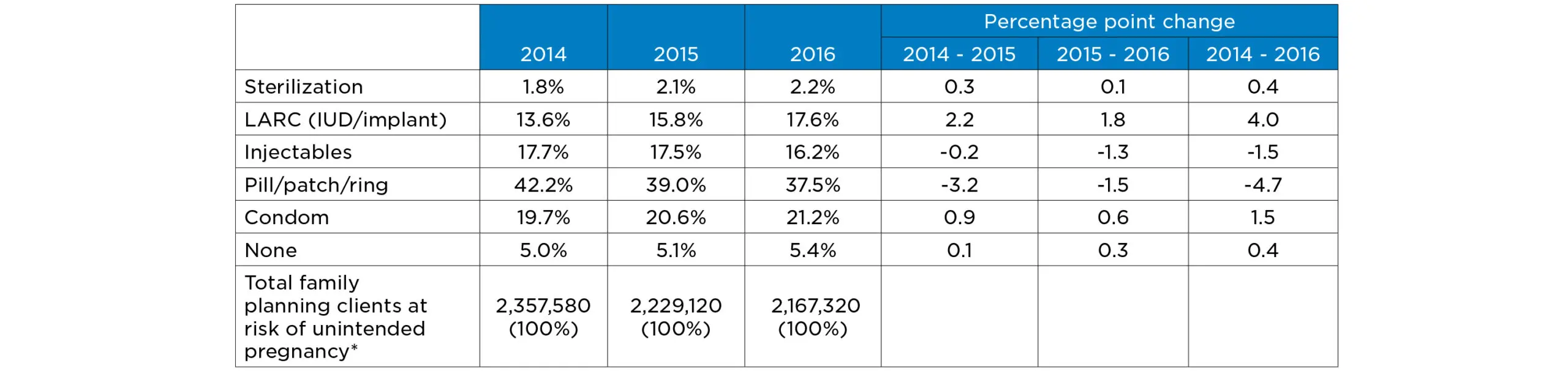
Source: Family Planning Annual Reports 2014 – 2016, Exhibit 18
*We exclude women who are abstinent or pregnant/seeking pregnancy. Numbers rounded to nearest ten.
Simulation results
We entered the contraceptive method distributions from each year into FamilyScape to estimate the potential change in the unintended pregnancy rate among Delaware Title X family planning clients and among Title X family planning clients nationwide, over time.
Figure 1 shows the estimated unintended pregnancy rate per 1,000 Title X family planning clients aged 20 to 39 who were at risk of unintended pregnancy (sexually active but not pregnant or seeking pregnancy), based on the contraceptive method distributions at Delaware’s Title X clinics and Title X clinics nationwide. In 2014, contraceptive method use among 20- to 39-year-old Title X family planning clients in Delaware was similar to that of Title X family planning clients nationwide; therefore, the simulated pregnancy rates for this population were also similar.
Among Title X family planning clients in Delaware, the estimated unintended pregnancy rate fell from 106.0 to 89.7 per 1,000 women between 2014 and 2016, or by approximately 15.4 percent. For Title X family planning clients across the country, the estimated unintended pregnancy rate fell from 106.6 to 105.3 per 1,000 women, or by approximately 1.3 percent.
Figure 1. Simulated unintended pregnancy rates, Title X family planning clients aged 20-39* in Delaware and the United States, 2014-2016
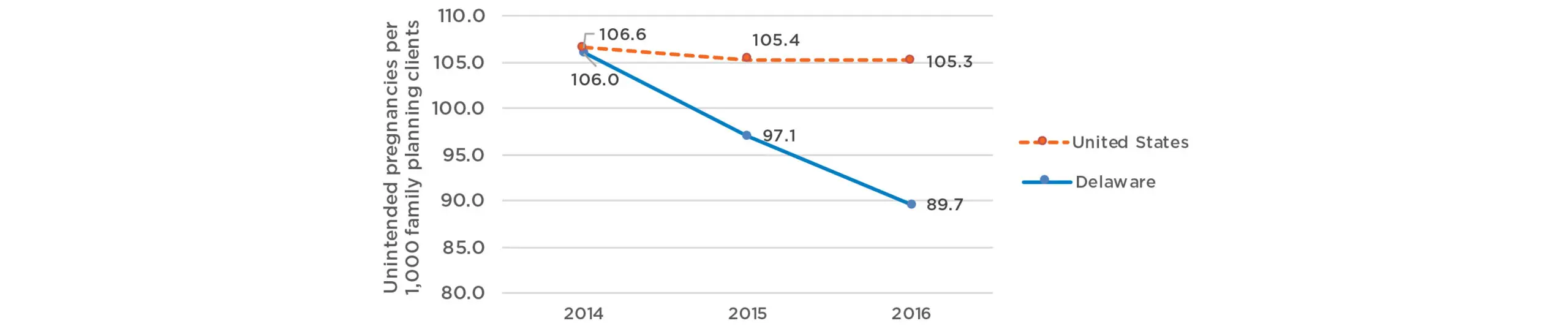
Source: FamilyScape simulations using state-level Title X data from Delaware and from U.S. Title X data, 2014-2016
*We limited our study to women at risk of unintended pregnancy (sexually active and not pregnant or seeking pregnancy)
Limitations
The primary limitation of this analysis is the quality of the statewide Title X data from Delaware:
- Delaware’s statewide Title X data are missing contraceptive method information for a large percentage of women. Among 20- to 39-year-olds at risk of unintended pregnancy, 43 percent were categorized as Method Unknown in 2014, and 27 percent were listed as Method Unknown in 2015 and in 2016.d These women were excluded from our analysis, and we assumed that the distribution of methods used by these women matched the distribution we calculated with the data available. If this is not the case, we could be over- or under-estimating the improvement in LARC use over time, as well as changes in the other method categories. However, comparing unintended pregnancy rates in 2015 to 2016 (fewer women were missing method data in these years), we found a reduction of 7.6 percent, similar to the 8.4 percent found between 2014 and 2015.
- Another limitation of the Delaware data is the high rate of incorrect method categorization among teens, which led us to exclude women aged 15 to 19 from our analysis.e This means our analysis does not account for approximately a quarter of family planning clients served by Title X clinics in Delaware.
- To ensure confidentiality, the data given to Child Trends by the Delaware Department of Health and Social Services were suppressed if a cell size (the number of women in an age group using a particular method) was between 1 and 10 (e.g., if 9 women aged 18 to 19 used a cervical cap, we would only know that this number was between 1 and 10). Most of these cells were for women in age groups outside of our age range of interest (20 to 39); however, there were several (less popular) method types for which we had to use an average estimate instead of using the exact number of women. In the end, however, we believe this small margin of error had little impact on our results.
With these limitations in mind, our FamilyScape analyses are useful for assessing the potential effect of Upstream’s Delaware CAN initiative. FamilyScape accurately models women’s contraceptive behaviors and the likelihood of pregnancy, by method; it allows researchers to efficiently estimate reductions in unintended pregnancy, when tracking actual pregnancy rates would be a more challenging and time-intensive process.
Conclusion
Based on 2014 to 2016 statewide Delaware Title X family planning data, there was a substantial increase in the percentage of women whose primary method was a LARC and a decrease in the percentage of women using the Pill, patch, or ring. The use of other methods stayed consistent, with a slight decrease in the use of no method between 2014 and 2016. This shift from moderately effective methods to highly effective long acting methods, along with a slight reduction in non-use, resulted in a considerable simulated decrease in the unintended pregnancy rate among Title X women, of 15 percent between 2014 and 2016.
To contextualize our findings in Delaware, we ran a similar analysis using national Title X clinic data. Nationwide, LARC use among Title X family planning clients increased by approximately 4 percentage points (from 13.6 percent to 17.6 percent). This was more than offset by decreases in the Pill, patch, ring, and injectables. Unlike in Delaware, the proportion of women using no method stayed consistent over time. Taking these changes into account, the estimated decrease in unintended pregnancy nationwide between 2014 and 2016 was 1.3 percent.
While we cannot explicitly attribute all of the changes in contraceptive use to Upstream, their work with Title X clinics in Delaware has coincided with a large increase in the use of LARC methods—a far more substantial increase than we estimated among Title X clinics nationwide. This improvement in contraceptive use is linked to a meaningful decrease in the simulated unintended pregnancy rate during this period, while the rate among nationwide Title X clients is estimated to have dropped less notably.
References
1. Finer LB, and Zolna MR, Declines in unintended pregnancy in the United States, 2008–2011, New England Journal of Medicine, 2016, 374(9): 843–852.
2. Dott M, et al., Association between pregnancy intention and reproductive-health related behaviors before and after pregnancy recognition, National Birth Defects Prevention Study, 1997-2002, Maternal and Child Health Journal, 2010, 14(3): 373-381.
3. Kost K, and Lindberg L, Pregnancy Intentions, Maternal Behaviors, and Infant Health: Investigating Relationships With New Measures and Propensity Score Analysis, Demography, 2015, 52(83).
4. U.S. Department of Health and Human Services, Healthy People 2020, Washington, DC: U.S. Government Printing Office, 2010.
5. Sawhill I, Karpilow Q, and Venator J, Improving children’s life chances through better family planning, Washington, DC: Brookings Institution, 2014.
6. American College of Obstetricians and Gynecologists, Increasing Access to Contraceptive Implants and Intrauterine Devices to Reduce Unintended Pregnancy. Committee Opinion No. 642, Obstet Gynecol, 2015, 126(e44-8).
7. Harper CC, et al., Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial, Lancet, 2015, 386(9993): 562-568.
8. Winner B, et al., Effectiveness of long-acting reversible contraception, New England Journal of Medicine, 2012, 366: 1998-2007.
9. AM B, and J. J, Trends in long-acting reversible contraception use among U.S. women aged 15–44, Hyattsville, MD: National Center for Health Statistics, 2015.
10. Institute G, State Facts About Unintended Pregnancy: Delaware, 2017.
11. Hack M, et al., Outcomes in young adulthood for very-low-birthweight infants, New England Journal of Medicine, 2002, 346(3): 149-158.
12. Sonfield A, Hasstedt K, and Gold R, Moving Forward: Family Planning in the Era of Health Reform, New York: Guttmacher Institute, 2014.
13. Fowler CI, et al., Family Planning Annual Report: 2014 National Summary., Research Triangle Park, NC: RTI International, 2015.
14. Fowler CI, et al., Family Planning Annual Report: 2015 National Summary, Research Triangle Park, NC: RTI International, 2016.
15. Fowler CI, et al., Family Planning Annual Report: 2016 National Summary, Research Triangle Park, NC: RTI International, 2017.
16. Vaughan B, et al., Discontinuation and resumption of contraceptive use: results from the 2002 National Survey of Family Growth, Contraception, 2008, 78: 271-283.
17. Guttmacher Institute, (2016), Fact sheet: Unintended pregnancy in the United States, Guttmacher Institute. Retrieved February, 9 2016, from the World Wide Web: http://www.guttmacher.org/pubs/FBUnintended-Pregnancy-US.html
18. Thomas A, and Karpilow Q, The intensive and extensive margins of contraceptive use: comparing the effects of method choice and method initiation, Contraception, 2016, 94: 160-167.
Acknowledgments
Upstream USA commissioned the research presented in this brief. The contraceptive use information for Delaware was provided by the Delaware Department of Health and Social Services, Division of Public Health, and contraceptive use information for Title X clinics across the United States was drawn from Family Planning Annual Reports prepared by RTI International and published by the Office of Population Affairs in 2014, 2015, and 2016. The FamilyScape microsimulation model used in this research was developed by The Brookings Institution and then expanded and updated to FamilyScape 3.0 by researchers at Child Trends, Georgetown University, and The Brookings Institution. We are grateful to Kristin Moore, Jody Franklin, August Aldebot-Green, and Carol Emig of Child Trends for their careful review and helpful comments and suggestions.
© Copyright 2024 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInThreadsYouTube