School-based Strategies to Support Adolescent Sexual and Reproductive Health
Schools—including high schools, community colleges, and universities—play a critical role in meeting the health care needs of youth. Currently, a wide range of health care services, including sexual and reproductive health care, are provided in school settings. In some high schools, students receive services on-site through school-based health centers (SBHCs), or through student health clinics on college and university campuses. However, not all school-based health service providers include sexual and reproductive health services, and others provide only a limited set of sexual and reproductive health services. There are also many schools (90% of high schools, 59% of two-year colleges, and 15% of four-year colleges) in which no health care services are available on campus.
This resource provides an overview of strategies that schools and school-based health service providers can use to better meet the sexual and reproductive health care needs of their students. Some of these strategies are already being used in school-based settings, while others could be adopted by schools seeking to expand their health services or those that currently do not provide any on-site health services.
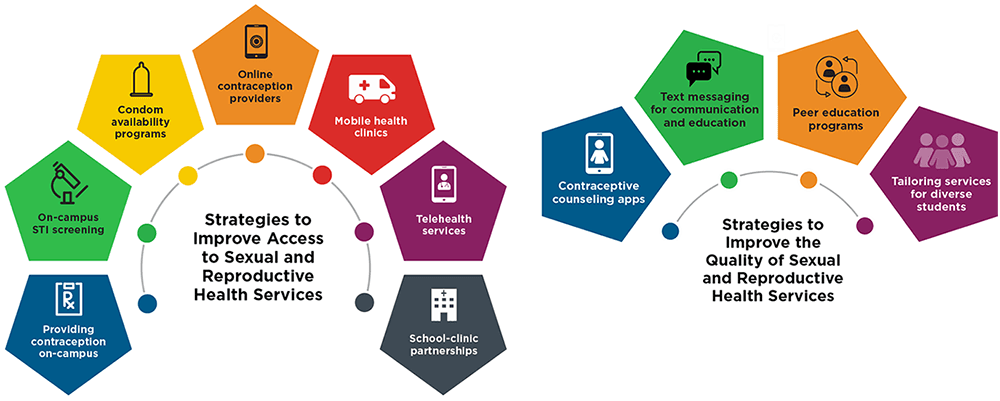
The strategies outlined in this resource include those that improve students’ access to sexual and reproductive health services and those that improve the quality of services being provided—often via youth-friendly approaches that better meet youths’ sexual and reproductive care needs. This resource additionally provides examples of how each strategy has been implemented in a real-world setting and presents considerations for each particular strategy.
The value of any particular strategy will depend on its context. For example, in a school with a health center that already provides prescription contraception on-site, it may be especially beneficial to integrate a mobile app to make contraceptive counseling more engaging and patient-centered. In contrast, schools that are committed to supporting the health care needs of their students but that lack on-site health service providers may benefit more from strategies that provide condoms to students or connect them with local health care clinics. Additionally, the most appropriate strategies will depend on the needs and resources of the populations being served. For example, reliable access to the internet and comfort with health service providers will determine clients’ use of certain strategies.
A note about COVID-19
The strategies highlighted in this resource were identified via a literature scan conducted prior to COVID-19. Many remain relevant during the pandemic. A separate brief highlights some key innovations that schools could adopt to provide sexual and reproductive health care in response to the pandemic.
To view a real-world example of each strategy and for further considerations, click on the text or plus sign where indicated.
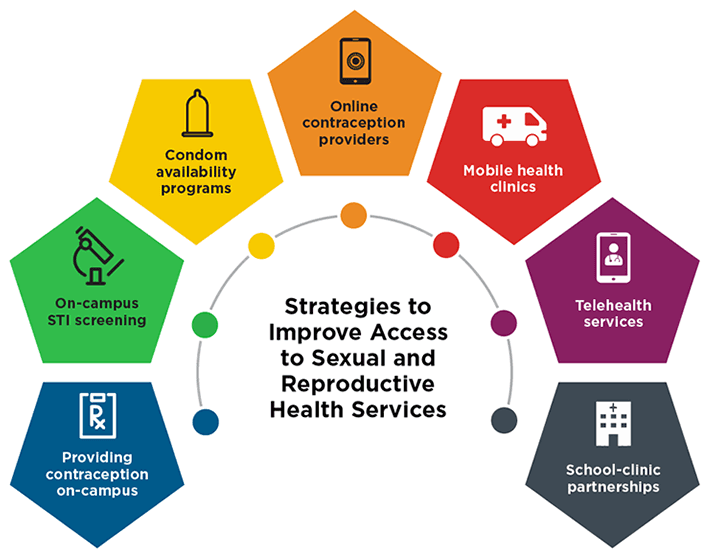
Students face multiple barriers to accessing sexual and reproductive health care services, including a lack of transportation or insurance, confidentiality concerns about using their parents’ insurance, and unfamiliarity with navigating the health care system. Schools can use some of the following strategies to promote student access to sexual and reproductive health services.

Many school-based health services—including those at some high schools and community colleges—provide a limited range of prescription birth control methods on-site, including oral contraceptive pills and Depo-Provera. Emergency contraception is also available in school-based settings, and some university student organizations even set up vending machines to dispense emergency contraception. Other schools are expanding their reproductive health services to include long-acting reversible contraceptive methods (LARCs), such as the IUD and implant, as these methods are the most effective reversible methods and are not prone to user error. Providing prescription contraceptive services on-site can reduce some common barriers to contraception for students, including limited awareness of where off-campus health service providers are located, lack of trust in sexual and reproductive health service providers, and lack of time or transportation to get to a clinic.
Example and Considerations

Youth ages 15 to 24 have among the highest rates of sexually transmitted infections (STIs) in the United States; when untreated, STIs can have serious long-term health consequences. Offering or expanding STI screening programs at schools can increase the number of students who receive testing and treatment for STIs by normalizing screening and integrating it into routine care. On-campus testing and treatment can help young people overcome barriers to receiving care, including those linked to transportation, cost, and comfort.
Examples and Considerations
Condom availability programs in schools and colleges can increase students’ access to condoms by providing them freely and in convenient locations. Although condoms are an effective method for preventing STIs and unplanned pregnancy, adolescents and young adults may be too embarrassed to purchase condoms or lack the money to do so. In practice, condom availability programs may look different depending on the particular school setting.
Examples and Considerations

Online contraceptive providers allow users to get a prescription for oral contraceptives, the contraceptive ring, patch, or emergency contraception without having to go to a provider in person. Depending on the service, users can have their contraceptive method delivered directly to their home or pick it up at a pharmacy. This service may be useful for students without on-campus health service providers. Additionally, online consults are often free or low-cost and allow for greater confidentiality, particularly for those living in small, rural communities who may worry about being recognized. Schools can help connect students with online contraception providers.
Example and Considerations

Mobile health clinics are customizable vehicles staffed by providers that travel to communities to provide health care services, including sexual and reproductive health services. They can readily provide condoms and hormonal methods of contraception; with some additional training of staff and resources, these vehicles can also provide LARCs. Mobile clinics can help provide reproductive health services at schools that do not have a health clinic (or that do not provide sexual and reproductive health services) or are located in communities with limited local sexual and reproductive health care providers. Mobile clinics at schools can help some adolescents overcome barriers to accessing care, including lack of time, lack of transportation, cost, stigma, and not knowing where clinics are located.
Example and Considerations

Telehealth, also referred to as telemedicine, uses technology to offer patients remote medical visits (not inside a physical doctor’s office or hospital), often via a real-time, two-way phone or video conversation. Telehealth may be a useful strategy to reach students at schools that do not provide sexual and reproductive health care services on site, or for students who live in communities with limited health care service providers. Even some students at schools with health service providers may find telehealth more convenient and comfortable. Telehealth has been an essential mode of health care provision during the COVID-19 pandemic.
Example and Considerations
Partnerships between schools and off-campus sexual and reproductive health service providers who share similar goals is a low-cost strategy to improve youth and young adults’ access to care. Partnerships can vary widely in practice, but common approaches include directly introducing the student to the partnering practitioner, having practitioners from nearby clinics visit schools, and offering a mobile health clinic on school grounds. These partnerships may be particularly useful for schools with resource constraints or those that are otherwise unable to provide services on site.
Example and Considerations
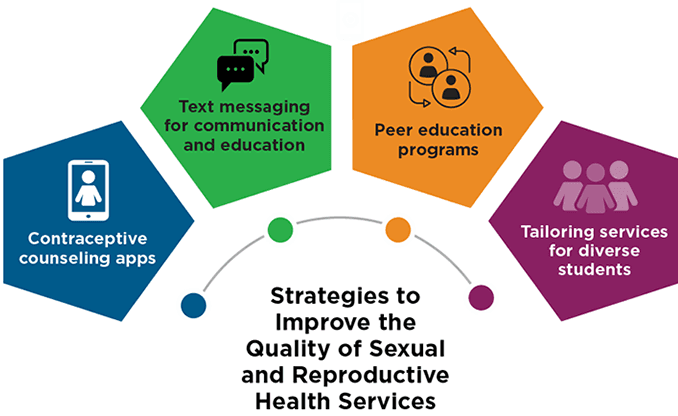
To meet students’ sexual and reproductive health needs, school-based sexual and reproductive health care providers must also consider the quality of their services and ensure that these meet students’ needs. Strategies to enhance the quality of sexual and reproductive health services for students include integrating mobile apps, using text messages to reach students, establishing peer education programs, and tailoring services and service settings to meet the needs of specific populations.

Numerous apps are designed for adolescents and young adults to use in a clinic waiting room, and typically allow users to filter contraceptive options based on their lifestyle and preferences. Contraceptive counseling apps can be tailored for the needs of specific populations. For example, Hi52Hlth from Baylor Teen Health Clinic is tailored for adolescents who have received an HIV diagnosis, while Decide + Be Ready from the University of Southern California and the U.S. Navy is tailored for women in the military. Using an app to review information about contraceptive methods in the waiting room prior to a visit can help students feel more comfortable, prepared, and informed for their appointment. For providers, apps can save time and help overcome any discomfort discussing contraception.
Example and Considerations

Text messaging can be used by school-based health service providers to send students reminders about upcoming appointments; texts can also improve the consistency of students’ contraceptive use by reminding them to take their birth control pills daily, change their ring or patch, or come to the clinic for a Depo-Provera shot on time. Additionally, text messaging can enhance health education. Teens may find it difficult to absorb complex information within the time constraints of a short medical consultation; text messaging allows them to ask questions after a clinical visit. Text messaging also allows youth to confidentially seek personalized answers to questions.
Examples and Considerations

Peer education programs are commonly used to provide students with the opportunity to receive health education—including sexual and reproductive health information—from peers who share similar backgrounds, based on factors like age, gender, sexual orientation, or race/ethnic identity. Peer education is a youth-friendly approach that delivers information to students in a comfortable, relatable way and helps youth gain a greater ability to ask questions, particularly about sensitive topics such as sexual and reproductive health. Peer educators (also called “peer advocates”) may be recruited and trained by student organizations or by school-based health service staff. Volunteer peer education programs have been used by schools, including some minority-serving institutions, to help address notable disparities in sexual and reproductive health outcomes.
Example and Considerations

Improvements to the clinic environment and young people’s health service experiences—including interactions between health service providers and students—can increase the reach and effectiveness of care. This may be especially important for men, students from under-resourced backgrounds, and those who belong to groups that have faced a history of discrimination that has limited their ability to obtain appropriate sexual and reproductive health care in a non-stigmatizing way. For example, many LGBTQ youth have personal experience with LGBTQ-specific discrimination from providers, and school-based health services may not provide a genuinely inclusive environment. Incorporating programmatic and operational changes—like providing incentives for coming to the appointment (incentives could include cash, gift cards, movie tickets, or food), connecting patients to appropriate outside services, using a youth-friendly approach to inquiring about or discussing sexual histories, changing the waiting room area to promote greater inclusivity, conducting targeted outreach, providing staff training, and implementing tailored services—may allow school-based health service providers to better reach and engage with the full diversity of students at their school.
Example and Considerations
Methods
From October 2019 to February 2020, we conducted a literature search to identify the range of strategies being used (or that could be used) to deliver sexual and reproductive health care services in school-based settings—specifically in school-based health centers (SBHCs) and on community college campuses. Within these settings, we searched for some pre-identified domains of innovation (e.g., telehealth, technology, mobile clinics, and partnerships) and for some specific areas of reproductive health care services (e.g., sexual health, LARCs, contraception, Title X). Additionally, we included search terms to identify any additional approaches for reaching and providing services to underserved populations (e.g., hard-to-reach, youth-friendly). For these searches, we included strategies used in four-year historically Black colleges and universities (HBCUs) and Hispanic-serving institutions (HSIs), as well as those used outside of a school-based setting.
In total, we conducted 149 unique searches in Google Scholar and Google. We originally identified 282 resources (219 journal articles and 63 news articles and webpages), although some were added after the original scan was complete (for example, identified in the references of an existing article), bringing the total to 298. Notably, we found substantially more literature on sexual and reproductive health service delivery in high schools than in community colleges. Only a subset of the articles identified described strategies that were implemented (i.e., many articles suggested strategies, but did not describe their implementation). Thus, after concluding our initial search, we abstracted information from 108 resources (80 journal articles and 28 news articles and webpages), including details (when possible) on the specific strategy/innovation used, the population served, the setting, geographic location, evidence of effectiveness, and any barriers to implementation identified.
For this web-based tool, we first identified the most common domains of strategies for providing school-based reproductive health services within our body of literature. In addition to the pre-identified domains, we identified some new domains (e.g., onsite contraceptive services, texting, peer education). We organized the abstracted information by domain and synthesized the information within each domain. Within each domain, we highlighted one “real-world” example from the literature. To select these examples, we prioritized articles on interventions that were conducted in school-based settings (as opposed to those that could be adapted for school-based settings) and included sufficient information to adequately describe the innovation. In some cases, we highlighted two real-world examples within one strategy, either to illustrate the range of examples or to combine information to provide a more robust example.
Acknowledgements
The authors would like to thank Dr. Jennifer Manlove and Dr. Jenita Parekh for providing feedback on this product throughout its development. The authors would also like to thank Dr. Mindy Scott at Child Trends, Dr. Ana Caskin at MedStar Georgetown University Hospital, Callie Koesters at the Office of Population Affairs, and Emily Baldi and Suzanne Mackey at the School-based Health Alliance for their expert reviews of this product. The authors are also grateful to Anushree Bhatia, Melissa Perez, and Ambika Mathur for their research support, and Catherine Nichols, Stephen Russ, and Brent Franklin for their design and editing work. This publication is funded by grant number 1 FPRPA006065-01-00 from the Office of Population Affairs in the U.S. Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of OPA or HHS.
© Copyright 2024 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInThreadsYouTube


