
Toolkit for Improving Family Planning Services in School Settings
Methods
In Year 1 of the study, the Child Trends team interviewed staff in 48 school-based health initiatives across the United States that employed innovative approaches to serving high-need populations with family planning services. Child Trends and School-Based Health Alliance (SBHA) reviewed the sites interviewed in Year 1 to identify sites well suited to a deeper exploration of their innovations. We selected the innovative program sites described in the case studies through a site selection process that considered six factors. Specifically, Child Trends and SBHA identified the following six criteria, adapted from the National Implementation Research Network’s (NIRN) Hexagon Tool, to help us select sites for case studies:
- Need: site targets a population with high need
- Content: site focuses on an innovation related to family planning services
- Applicability: whether other programs would understand or be able to implement the model potentially
- Evidence: site collects data to describe the center’s reach or quality
- Willingness: site wants to participate
- Capacity: site is able to host a process evaluation
Sites that met all these criteria were selected for further review (i.e., they had high need; they had a family planning-focused intervention; their model was applicable to and replicable in other settings; they had some evidence for their model; they were willing to participate in a site visit; and they had the capacity to host a process evaluation). All the sites had innovative interventions (the criteria for a Year 1 interview), but replicability, geographic diversity, variation, and willingness were prioritized. The Child Trends team then gauged each site’s interest and capacity to participate in a virtual site visit (e.g., a set of interviews with key staff). A final list of interested sites included approximately 10 programs; Child Trends staff, with input from staff at SBHA, selected four with a priority on variation in their interventions, geographic location, and sponsor diversity. For example, we included one east coast site, one west coast site, and two sites from the Midwest. One site was a city health department, one was a local community clinic, and two had relationships with bigger hospital systems. Their interventions varied from one focused on health educators, to one that focused on school-based links to external clinics, to one that focused on how to make LARC insertions more accessible and less frightening, and to one hospital that partnered with local schools. Each of the interventions provided an interesting and replicable example from which other school-based health centers or staff in schools or clinics who want to work more collaboratively might learn.
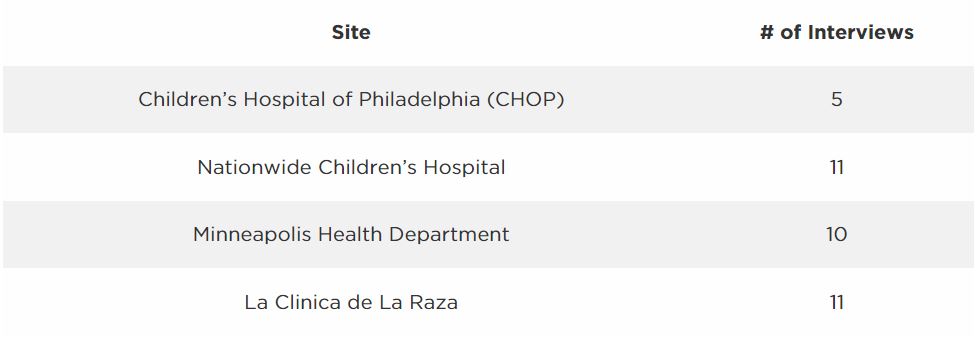
Once the four sites were chosen, Child Trends created teams of two to three people to lead each virtual site visit. They developed protocols, worked with site leaders to identify who to interview to gain a full perspective on how the intervention was developed and implemented, and analyzed the interview data. We worked with each site to identify the appropriate number of interviews (see table below):
Analyses were done using an informal coding approach so that themes were identified after each interview and then asked about in subsequent interviews until a clear narrative emerged. Then each case study identified those themes and the ways each site engaged in work around the four “foundational approaches” identified across sites. The themes identified in each case study focused on key recommendations for replicating the given intervention. While each intervention was different, the goal was to share lessons learned about what made the implementation of each intervention work and how others might learn from each site’s experiences.
© Copyright 2024 ChildTrendsPrivacy Statement
Newsletter SignupLinkedInThreadsYouTube